
Everyone likes to help and advise an expectant mother, and that’s a good thing. It comes from a good place. But it helps to study the facts for yourself, so you can make the best decisions possible for you and the baby. In fact, I wish more health care providers would do just that – arm us with facts instead of arbitrary rules. Many ultimatums are too broad, or not supported by evidence.
Now, if you choose to place full confidence in a trusted doctor or midwife and just do whatever he recommends, great! That’s certainly one acceptable approach. But if you’re interested in becoming more informed so you can take part in the decision-making process, read on!
Rule 1: Sleep on Your Left Side
There are entire threads on the internet about this one, and the question is often phrased like so: “Is it safe to sleep on my right side?” This immediately sets the stage for worry and anxiety. It just goes to show how strongly women have been indoctrinated into the “left is best” camp. With past pregnancies, I would awake in the night fearful that I’d hurt the baby simply because I’d rolled onto my back. But is sleep during pregnancy really that potentially hazardous?
THE FACTS: A few studies have found only a slight difference in blood flow when lying on your back versus your side. One of these studies pertained only to pregnant women undergoing surgery; the other didn’t give any instruction at all based on its findings. (1,2)
More recently, Canadian doctors Dan Farine and Gareth Seaward acknowledged that “Pregnant women who lie in a supine position may develop syncopal symptoms. However, of those women who become symptomatic, only 2% to 4% have significant aortocaval compression. Even in this small minority of symptomatic women, there is no evidence of fetal compromise. The advice often given to pregnant women to lie on the left side is therefore not relevant.” (3)
CONCLUSION: Good sleep is an elusive dream that slips away to near oblivion as your due date approaches. Who cares how or where you decide to sleep – the goal is to just get some rest! Your body is very smart. If the baby pushes on your bladder, you wake up and go to the bathroom. If you try to lie flat on your back, or wake and find yourself that way, it’s very uncomfortable, and you change positions. Problem solved.
Rule 2: You Don’t Have Many Pain Relief Options
The aches and pains of pregnancy are due to a myriad of factors. Your joints, your back, your head, your feet, sometimes even your veins (varicose!) can all experience pain for different reasons leaving you diligently searching for a natural anti-inflammatory for pregnancy. Beyond taking acetamenophen, there’s not much else that expectant mothers are advised to try besides non-medicinal measures like massage, and hot/cold packs.
THE FACTS: Thankfully, nature does offer some more options to ease your suffering. If you need a safe and effective and natural anti-inflammatory for pregnancy, topical pain relief is at hand. For an aching back, sore joints and legs and feet or even a superficial headache, formulations that contain natural ingredients like arnica and time-released menthol and camphor can be very effective. Doctor Hoy’s is a great source for targeted, natural pregnancy pain relief. They do not contain parabens, toxins, or aspirin derivatives.
It’s difficult to adequately study medications for safety in pregnant women, so it’s good to keep a safe and natural anti-inflammatory on hand for any aches and pains during and after pregnancy.
For lessening the pain and pressure of varicose veins, health care providers have also found that supplements like Vitamin E, stinging nettle, bilberry and bayberry can make a big difference.
CONCLUSION: Look into natural pain relief options that are well studied and safe for pregnancy. Check with your doctor or midwife about proper dosing.
Rule 3: You Should Switch to Decaf
Firstly, a full disclosure: I’ve been an avid black coffee drinker since the age of twelve. This is a myth I really wanted to debunk. 
THE DATA: There still isn’t any conclusive medical evidence that drinking a few cups per day will harm the fetus. By that I mean the studies we have are limited in scope, and don’t fully factor in other variables. Just to point out one obvious hole: researchers are not willing to have one group of pregnant women drink no coffee and another group drink 6-8 cups per day (surprise, surprise). In fact, you’d be hard pressed to find anyone, let alone an expectant mother, who drinks that amount! The only control group that did ingest high doses of caffeine for the sake of science was animals. And only then were scientists able to document a possible causal relationship between caffeine and problems like miscarriage and brain development.
The few studies that do show a possible link between miscarriage and “substantial” amounts of coffee in early pregnancy are not conclusive either because you can’t prove it isn’t just a correlation rather than a case of direct cause. Why? Because women who tend to drink more coffee also tend to be (a) older and (b) moderate to heavy consumers of alcohol and/or tobacco. All three are known risk factors for negative outcomes.
Another interesting fact: women who are more nauseated in early pregnancy tend to avoid or limit their coffee intake. And there is a link between more nausea and a lower incident of miscarriage. So, again, the slightly higher rates of miscarriage for moderate to heavy coffee drinkers could very well be due to the fact that these pregnancies were already doomed, and maybe that’s why the mothers weren’t feeling very nauseous, or even sick at all (4).
CONCLUSION: The data we currently have does not preclude enjoying a few cups per day. The current (American) recommendation of no more than 200 mg per day is arbitrary.

Rule 4: You Have to Get Antibiotics for Group B Strep
The Group B Strep question is a classic risk vs. benefit calculation, and yet almost never is it presented to pregnant women this way. Not only do we assume we have to take the test (we don’t), we are told IV antibiotics during labor are the best choice in event of a positive test (not necessarily). Nearly one third of pregnant women will be given antibiotics during labor; that’s a huge number, and certainly worth giving a second look.
THE FACTS: First of all, what is the theoretical risk posed by not treating Group B? I’ll use some Canadian research to give you a general idea. Of about 20% of women who tested positive and were untreated, 50% passed GBS on to their newborns. Roughly 49% of those colonized infants experienced zero symptoms. Between 1-2% actually developed early-onset GBS.
While nearly every doctor spends time talking about Group B risk, they collectively fail to educate women about the drawbacks of routine IV antibiotics for mother and baby, drawbacks which are are more likely to occur than actual GBS in the infant. Some of these negatives include:
- Increased risk of maternal and fetal candida/yeast infection (happened to me twice)
- Increased risk of breastfeeding problems, including giving up on breastfeeding (happened to me twice)
- Increased risk of labor complications due to the mother’s mobility being limited by the IV apparatus
- Negative effects on your baby’s microbiome, for up to one year, including (ironically) higher levels of harmful bacteria like Clostridium, Enterococcus, and Streptococcus (this happened to both of my sons in their first year). Possible links to childhood allergies and asthma are also being looked into.
- Routine use of antibiotics in healthy mothers and infants can lead to antibiotic resistance, a growing problem in our age. In fact, some of the antibiotics used in labor specifically for “treating” Group B Strep are resistant and ineffective (this particular study is over 10 years old, and the numbers continue to rise).
Quoting from an excellent assessment from Jane Sheppard: “By CDC estimates, we save the lives of two in 10,000 babies-0.02 percent-by administering antibiotics during labor to one third of all laboring women. We should also keep in mind that this figure does not take into account the infants that will die as a result of bacteria made antibiotic-resistant by the use of antibiotics during labor-infants who would not otherwise have become ill. When you take that into account, there may not be any lives saved by using antibiotics during labor.”
Apparently, mortality from GBS remains the same whether or not antibiotics are given. Less babies get sick, but death rates are not changed.
Routine antibiotics aren’t the only problem; the test itself is flawed. Colonization of Group B is very transient. You can test positive at 37 weeks and then be negative at 39 weeks, or vice versa. That means both missed colonizations and misdiagnosed colonizations. In one study, 9% of women who were tested at 35 weeks came up negative and were not given antibiotics during labor. They were tested again during labor and found to be positive. The same study showed that 16% of women tested positive at 35 weeks, but negative during labor. They were thus put on high-powered antibiotics for no reason.
A more recent study from 2009 showed that most cases (61%) of GBS in full-term babies happened with pregnant mothers who had been screened but tested negative. Yet our current testing system is treated like the gospel truth.
There’s also the fact that despite following all the doctor-approved protocols, women who test negative, and their babies, can contract Group B from the hospital itself!
CONCLUSION: Decision-making would be much easier if we had faster, better test results. Some doctors are even administering a simple blood test on the newborn with promising results.
In the absence of that, you have four options right now:
- Use the universal approach and take the antibiotics. Be open-minded about the possible negative side effects of this high-powered dose of medicine on both you and your baby in the short and long term.
- Use the risk-based approach. IV antibiotics are a reasonable choice if: you tested positive AND one of these three factors is present – pre-term labor, fever during labor or membranes that have been ruptured for 18 hours or more.
- Decline antibiotics if you test positive and take steps in the weeks before labor to encourage the colonization of good bacteria. Consider the Hibiclens protocol during labor as an alternative approach (studies are mixed on this one, but here’s some research on that). Other preventative measures include refusing unnecessary internal exams, refusing a membrane sweep, declining internal monitoring except when absolutely needed, avoiding induction or use of “ripeners” which are applied to the cervix, and not permitting the artificial rupture of your membranes.
IMPORTANT: Do not let a hospital give you the “he or me” routine, and threaten that either you or your baby MUST be given antibiotics. You have every right to say NEITHER, and it will not affect your insurance.
Rule 5: Someone Else Should Take Care of Your Cat
An avid cat lover, I was both scared and saddened when reading during my first pregnancy that someone else should take care of our cats because of a deadly pathogen called Toxoplasmosis.
THE FACTS: The risk of having Toxoplasmosis pathogens in your indoor cat’s litter box is statistically miniscule. A European multi-city study done in 2000 concluded “Contact with cats was not a risk factor.” Toxoplasmosis infection is most likely to be transmitted via undercooked meat and contaminated soil, not your cat. Furthermore, an infected cat only secretes the toxin for about 2 weeks, and how likely is it that those two weeks are going to fall during your pregnancy?
Two other things to be aware of. You might have already gotten the illness before conception, especially if you were around cats or spent a decent amount of time outdoors in your youth. Many don’t even know they had it because the symptoms range from unnoticeable to mild. And once you’ve had it you’re immune for life. You can even do a blood test before or during pregnancy to satisfy your curiosity.
CONCLUSION: Obsessing about our pet cats during pregnancy is unnecessary. Don’t eat undercooked meat and wash your hands after digging around in the soil, or changing the litterbox. Just common sense.

Rule 6: It’s Risky to Have a Baby After 35
I’ve conceived at 36, 37, 39 and 42 (among others!) so this one is near and dear to my heart. People tend to see age 35 as a big risk threshold that women should only cross with caution. Fueling this fear, many OB doctors automatically slap the “high risk” label on you if you’re over 35, setting the stage for undue anxiety and worry throughout the pregnancy.
What about all those statistics showing that women over 35 have a greater risk of problems and complications?
THE FACTS: First of all, understand that the risks increase very very slowly over time; it’s not like you hit 35 and all of a sudden you’re a walking time bomb. See how slowly that line creeps up? And see how low the percentages actually are? (it’s not even 1 percent at age 38)
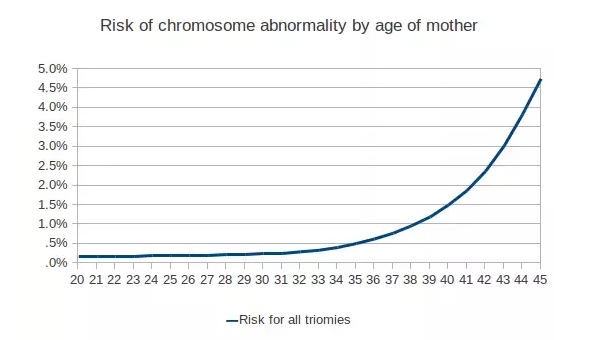
Take Down Syndrome, for one example. Dr. Sears says “Depending on how they are presented, these figures can be scary. If a doctor says to a mother, ‘At age thirty-five you have five times the chance of having a Down Syndrome baby than you did at age twenty,’ that would scare many senior mothers from conceiving. Here’s how I present the risk factors to my patients who ask. At age twenty you had a 99.95 percent chance of not delivering a baby with Down syndrome; at age thirty-five your chances of not delivering a baby with Down Syndrome are 99.75 percent. Doesn’t that figure sound more reassuring?” Maybe they shouldn’t even start to make a deal about risks until 45 or later. But even at age 45 you still have a 97 percent chance of delivering a baby without Down Syndrome.”
CONCLUSION: There’s no reason to worry about conceiving at age 35, or after. Not only do the majority of “risks” that we associate with advanced age increase extremely slowly over time, but our ability to do something about them is close to zero.
For more fact-based information about your pregnancy, check out these two great books – Expecting Better and Debunking the Bump!

Other Sources (Not Hyperlinked):
(1) Kaupilla, A.J.I, et al (1980). Decreased Intervillous and Unchanged Myometrial Blood Flow in Supine Recumbency. Obstetrics & Gynecology, The Effect of Lateral Tilt on Maternal and Fetal Hemodynamic Variables. Obstetrics & Gynecology, 77(2):201-3. DOI: 10.1097/00006250-199102000-00007
(3) Farine, D. and Seaward, G. (2007). When it Comes to Pregnant Women Sleeping, Is Left Right? Journal of Obstetrics and Gynaecology Canada, 29(10): 841-842. DOI: 10.1016/S1701-2163(16)32633-0
(4) Lawson CC, LeMasters GK, Wilson KA (2004). Changes to Caffeine Consumption as a Signal of Pregnancy. Reproductive Toxology, 18:625-33
(5) Abrams, B. et al (2000. Pregnancy Weight Gain: Still Controversial. American Journal of Clinical Nutrition, 71 (5 Suppl):1233S-41S. DOI: 10.1093/ajcn/71.5.1233s
(6) Schack-Neilsen, L. et al (2005). Gestational Weight Gain in Relation to Offspring Body Mass Index and Obesity From Infancy Through Adulthood. International Journal of Obesity, Severe Obesity, Gestational Weight gain, and Adverse Birth Outcome. American Journal of Clinical Nutrition, 91(6):1642-8. DOI: 10.3945/ajcn.2009.29008
Oster, E. (2013). Expecting Better: How to Fight the Pregnancy Establishment with Facts. New York: Penguin Press
Adler, D. (2014). Debunking the Bump: A Mathemetician Mom Explodes Myths About Pregnancy. (n.p.): Author
My thanks to Responsival who partnered with me on this post!
Oh wow! This is such interesting info. I was always told that I shouldn’t have coffee. I had a friend who was almost convinced by her doctor to give her cat away! Thank goodness she didn’t.
Giving up coffee is something that I could never do and couldn’t even manage to try during either of my pregnancies. I limited my caffeine of course and even opted for half calf some days, but I agree that there’s nothing wrong with it.
I had such a hard pregnancy with my first child. I had given up caffeine as soon as I found out I was pregnant and boy, was it hard!!
When my sister was pregnant the first time, she believed a bunch of these you have listed. By her third, she was a total mom pro!
I hate that there are so many myths out there about pregnancy. With education it’s pretty simple to tell what is a myth and what isn’t luckily.
This is a ton of great info! I’m a huge believer that knowledge is power and I love that you’re empowering women to make sound decisions for themselves and their babies!
I totally bought into the sleeping on your left side thing! I think partially because I felt better on my left, but too funny! If I’m ever nauseous now, I feel slightly better on my left side. Weird?
It’s the opposite for me; my tummy feels unsettled when I’m on my left, so I rarely sleep that way. Of course, when I turn to the right, I get heartburn. Can’t win! LOL
Oh yes! I remember some of these myths. I remember that I didn’t drink any coffeee and I couldn’t plan any trip by airplane. I am so glad that these are only myths
This is really helpful! Thank you so much for sharing these!